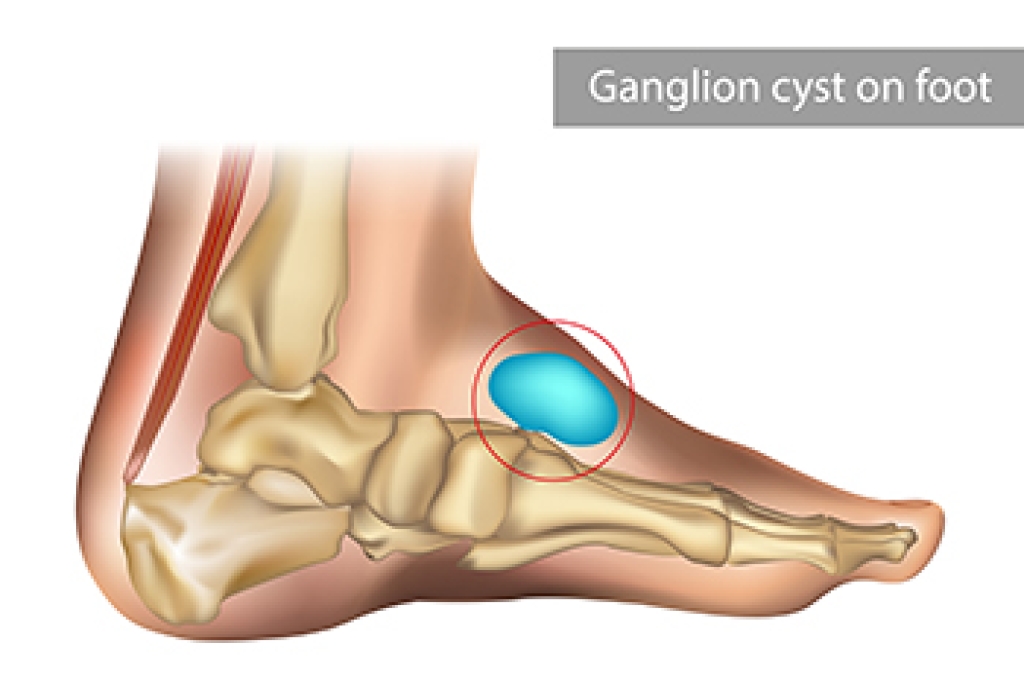
A ganglion cyst on the foot is a small, soft, fluid-filled sac that usually develops near a joint or along a tendon sheath, most often on the top of the foot. The lump may feel movable beneath the skin and can change in size over time. Many ganglion cysts cause no discomfort, while others produce aching, burning, or pressure pain when a shoe presses against the area or during activity. Although generally harmless, the mass may interfere with walking or shoe comfort. The exact cause is uncertain, but prior injury, repetitive stress, and joint irritation are commonly associated factors. A podiatrist can evaluate the lump, confirm the diagnosis, and rule out other conditions with imaging when necessary. Treatment options include protective padding, pressure relief, fluid aspiration, or surgical removal. If you have an unexplained lump on the top of your foot, it is suggested that you make an appointment with a podiatrist for an exam, diagnosis, and treatment.
Foot Pain
Foot pain can be extremely painful and debilitating. If you have a foot pain, consult with Andrew Katz, DPM from Allcare Foothealth Center. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Causes
Foot pain is a very broad condition that could be caused by one or more ailments. The most common include:
- Bunions
- Hammertoes
- Plantar Fasciitis
- Bone Spurs
- Corns
- Tarsal Tunnel Syndrome
- Ingrown Toenails
- Arthritis (such as Gout, Rheumatoid, and Osteoarthritis)
- Flat Feet
- Injury (from stress fractures, broken toe, foot, ankle, Achilles tendon ruptures, and sprains)
- And more
Diagnosis
To figure out the cause of foot pain, podiatrists utilize several different methods. This can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatment depends upon the cause of the foot pain. Whether it is resting, staying off the foot, or having surgery; podiatrists have a number of treatment options available for foot pain.
If you have any questions, please feel free to contact our office located in Palmdale, CA . We offer the newest diagnostic and treatment technologies for all your foot care needs.